We talk a lot about healthcare costs. But what about the silent one building up every night? Sleep deprivation is one of the biggest unspoken drivers of MSK issues, chronic pain, workplace burnout – you name it. From slower reaction times to more sick days, sleep debt builds up…and healthcare pays for it.
You can stretch, ice, and strengthen… but if you’re not sleeping, you’re not healing.
I used to think recovery was about reps and routines. But then I started looking at recovery data. The real magic it turns out, happens at night. Tissues repair. Inflammation reduces. Pain signals recalibrate. All while you sleep. But here’s the problem: pain disrupts sleep. And poor sleep increases pain sensitivity. It’s a vicious cycle.
Pain and sleep have this toxic relationship: pain makes it harder to rest, and poor rest makes pain feel worse the next day. It’s not just about being tired. Poor sleep delays healing, slows muscle repair, and increases inflammation. And here’s the thing: many people don’t even realise sleep is the problem.
Lack of rest weakens recovery, heightens pain perception, and drains productivity.
It’s no surprise absenteeism and insurance claims are higher among poor sleepers.
I’ve seen workplaces throw money at standing desks and gym passes, but ignore the sleep problem.
Research suggests that sleeping 7 to 8 hours per night is associated with the lowest risk of absence from work due to sickness. Or to be precise: 7 hours, 38 minutes for women and 7 hours, 46 minutes for men. Results show that the risk of an extended absence from work due to sickness rose sharply among those who reported sleeping less than 6 hours or more than 9 hours per night.
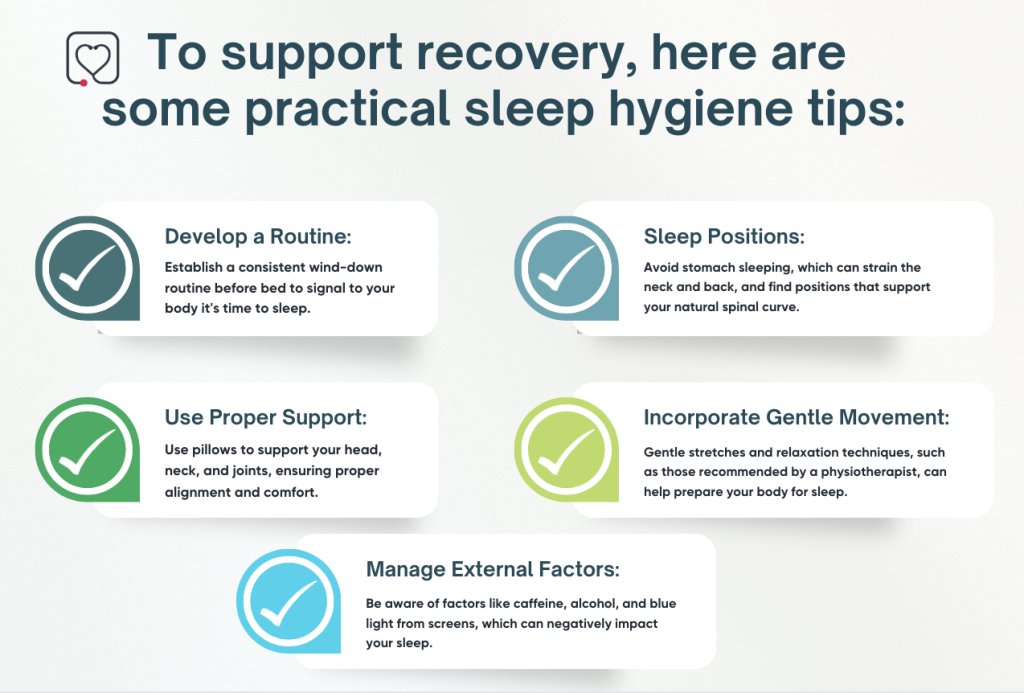
At DocHQ, we’re starting to integrate sleep education into MSK pathways. Because pain management and sleep hygiene are deeply connected. Whether it’s posture during sleep or stress from pain interrupting rest—it all feeds into how we recover. If we want stronger healthcare systems, we need to treat sleep like medicine. It’s not optional. It’s foundational.
That’s why we don’t just track exercises – we monitors patterns. We’re working with partners to include sleep screening in MSK assessments – because movement and rest go hand in hand.
If someone’s progress is stalling and pain is persistent, sleep issues are often the clue.
And when we flag that early, clinicians can adjust routines, recommend better wind-down strategies, or even intervene clinically.
Tips for Sleeping Better
Learn more: https://www.youtube.com/watch?v=07swJHnllMU&list=PLMKIb8FpgoAEZYxP_O_gYL01gmm1D9Rll&index=1



